This is part three, and the final part, of my infertility catch-up series. Part one covers the beginning of our journey, what we tried before getting the official “infertility” diagnosis, and necessary medical background to understand the process (a detailed rundown of the menstrual cycle and how conception occurs). Part two continues with our journey and catches you up with all the testing we did the last half of 2018. Part two includes doctor changes, lots of blood tests, and lots of imaging.
This part, part three, will go into the details of what the infertility testing showed and what those results mean. I also give a list of the supplements that Dan and I have both started on the advice of our fertility clinic. This supplement list is for informational purposes only, and will never include dosages. If you’re interested in the supplements, please talk to your own doctor.

Remember, every person dealing with infertility has a unique experience. All human bodies are different. What works or doesn’t work for you will be totally different from the next person you talk to, even if you have the same condition. Keep that in mind going through this series. Also, my test results and their interpretation are likely different from yours; every clinic has its own ideas of where these numbers should fall. Make sure you trust your clinic and your doctor!
I am not a doctor. This post is not medical advice. Do not change any aspect of your healthcare, without consulting any of your medical team, due to the content of this post. If this disclaimer is ignored, I cannot be held liable for any harm you may cause yourself.
My Testing
Prolactin
The first test I had related to fertility was a prolactin test in February 2018. My prolactin was 16.8, which is completely normal. Prolactin levels that are too high can impeded ovulation because your body will think you’re pregnant.
October 11, 2018: Prolactin was 36.2, while the upper limit for “normal” is 23.3, but the doctor said it could be due to not fasting (and they’re unsure as to the exact mechanism behind this).
October 24, 2018: Fasting prolactin was 25.1. This is still too high, but not high enough to require treatment or any further testing. I had no symptoms of elevated prolactin (I was ovulating and having regular periods).
January 28, 2019: The clinic wanted to recheck the prolactin to make sure that my levels weren’t rising. My prolactin was 13, which is exactly where it should be. No idea why they were elevated for a little while, but at least they’re normal again. (The Pituitary Society says prolactin can be elevated due to stress, and I was definitely stressed in October. So, maybe?)
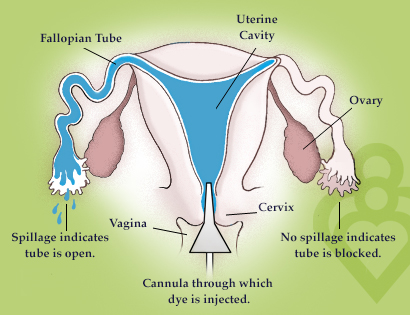
HSG
This was performed in July 2018. You can read more details about it in this post. The HSG showed my uterus is a normal shape and that my Fallopian tubes do not have any obstructions. My current clinic is a little confused about why one of my tubes appears to be in an unusual location, but for now that is not a concern. The doctor did mention possibly repeating the test if I continued to struggle with conceiving.
Progesterone
My OBGYN checked my progesterone on cycle day 21 to help determine if I was actually ovulating. At the time, I was doing a progesterone topical cream that was over-the-counter. On CD21, which was October 1, 2018, my progesterone was 21.8. I was told this was a great number and it looked like I was indeed ovulating and I did not need to supplement my progesterone. I thought they remembered my cream, but I think they probably didn’t (based on what I’ll say next).
The fertility clinic (AWC) likes to get two post-ovulation progesterone checks. They checked my progesterone levels on December 21st and December 24, 2018. I was no longer doing anything to supplement my progesterone. December 21st, my progesterone was 16. December 24th it was 6.1. They prefer those numbers to be 20 and 10. This means, my body [barely] does not make enough progesterone on its own.
Thyroid
The doctors have done a full thyroid panel on me. I’ve had various values checked many times before, so they decided to get more recent numbers. Thankfully, my thyroid values have always been normal for every test. My TSH levels are even alright in the narrower range used for fertility and pregnancy. (My dad had Grave’s Disease, until they nuked his thyroid, so I am vigilant about getting my thyroid checked.)
Estrogen
Estrogen is an important hormone for the menstrual cycle (which I talk about more in part one). The blood test is technically called “estradiol,” which is a specific form of estrogen. My OBGYN ran the test on October 11, 2018 (CD3), and my estradiol was at 29.5, which is normal. The fertility clinic wanted to recheck it on CD3 after some of my supplements had been started. On December 6, 2018, my estradiol was at 46.6 which I was told was “totally normal.”
Testosterone and DHEAs
While testosterone is often thought of as a “male hormone,” it’s important in female bodies as well (which I also talk more about in part one and in this post). The ovaries use testosterone to create estrogen. DHEAs are another type of testosterone in our bodies.
November 26, 2018: Testosterone was 30 and DHEAs were 223.9. While these levels are “good” according to LabCorp, they’re lower than the fertility clinic likes. The fertility clinic prefers to see testosterone between 50 and 100, and DHEAs between 300 and 500. To make up the difference, I was started on a supplement to help raise my testosterone levels.
December 10, 2018: Testosterone was 120 and DHEAs were 936.7. Whoops! Those went too high, so the supplement was adjusted.
December 21, 2018: Testosterone was 71 and DHEAs were 616.4. While the DHEAs were technically a little high, the clinic was happy with my numbers. I’m to continue the supplement at its current dose until I’m told otherwise.
FSH and LH
Follicle stimulating hormone (FSH) is the hormone that tells your ovaries to start to mature some eggs. Luetenizing hormone (LH) is the hormone that tells your ovaries to release an egg (ovulate). Both of these hormones are present, at testable levels, between CD1 and the time you ovulate. On December 6, 2018, my FSH was at 5.5 and my LH was 3.5 – both normal.
AMH
Anti-mullerian hormone (AMH) is a hormone that is used as an indicator of ovarian egg reserve – essentially, how old your ovaries are. (I talk more about AMH in this post.) While mine was “normal,” at 1.97 (on October 24th), it was a lower number than they’d expect for a 28 year old woman. Because of this, they decided to retest it using a lab that specializes in female hormones. Unfortunately, that test came back even lower. While this by itself isn’t enough to get a diagnosis, it points towards diminished ovarian reserve – a fancy way of saying I don’t have as many eggs as I should at my age.
RFC
The resting follicle count (RFC) is an ultrasound. They use an ultrasound to look at your ovaries and count how many follicles you have around CD3 (between CD3 and CD5). When your ovaries start to mature eggs, they start with many follicles on each ovary. Once one of the follicles reaches a certain level of maturity, the other follicles die and your body focuses on the one that matured first. The RFC is used with the AMH to determine your ovarian health.

December 6, 2018: My right ovary had 17 follicles, which is exactly what they’d expect for a woman my age. My left ovary had 2 follicles, which is abnormal. Essentially, we discovered that my left ovary is doing almost nothing. With my left ovary only attempting to mature two follicles, it is unlikely I ovulate from it at all. Paired with the results from my AMH test, I think it means I have “diminished ovarian reserve.” (We have not talked to the doctor yet to confirm that diagnosis.) I was started on supplements specifically for diminished ovarian reserve.
January 28, 2019: My right ovary has 19 follicles, which is perfect. My left ovary has 6 follicles. While 6 follicles is still lower than it should be, I’m grateful that the number has increased and I’m hopeful that means that the supplements are working! Instagram post about this RFC can be found here.
Dan’s Testing
Semen Analysis
Since semen is the “end product” of the male reproductive system, and an easy test, they run this first. Dan’s numbers, on the first analysis, were “perfect.” He’s technically had one full semen analysis done, and a partial analysis. When they do the sperm wash for an IUI, they do another less involved semen analysis. The most important of the numbers is the “total motile count.” The total motile count is the amount of sperm that are actively swimming and have a chance to reach the egg.
July 2018: Dan’s total motile count was 94.71 million. To be “normal” it needs to be over 20 million. Obviously, this number is great!
October 2018: Dan’s total motile count before the semen wash for the IUI was 38.25 million. While that’s still over the 20 million, it’s less than half of what it was the first time. The steep decline (likely due to stress and lack of sleep) had AWC concerned, so they started Dan on supplements to help make his counts and quality as good as possible.
Because Dan’s semen analysis is exactly as it should be, there has been no need for Dan to do any further testing. Even the decline isn’t reason to pursue further testing at this time, especially since Dan and I are confident it was due to graduate school.
Treatments
Since I do not want people to change their medical care without consulting their doctor first, I will not include dosages for any of our medication/supplements. Please consult with your doctor if you feel these may be helpful for you. This is included for informational purposes only.

My Supplements
To help my ovarian and egg health, due to my diminished ovarian reserve, I was started on a long list of supplements. I was also started on a supplement due to my low testosterone and DHEAs levels.
- DHEA supplement (I started at a higher dose, determined by my doctor, and am now on a lower dose) – if you choose to ignore my disclaimer, do not ignore this: do NOT start this supplement without a doctor, too much testosterone can have dangerous effects in the body!
- Prenatal vitamin with folic acid – I’ve been on this since 2017, but AWC recommended a different one, so I switched.
- CoQ10
- Inositol (myo-inositol and d-chiro inositol)
- Vitamin D3 – I take one that also contains vitamin K2 to enhance absorption, on the advice of my dietitian
- Pyrroloquinoline Quinone (PQQ)
- Omega-3 (fish oil)
Dan’s Supplements
These supplements are to help boost the health of Dan’s semen/sperm. While his numbers are good, there’s no harm to taking these. Hopefully, boosting his numbers and quality as much as possible will help us conceive sooner. Dan does also take a fish oil supplement because my dietitian said it’s a good idea from a general health perspective, and I’ve done some research that it can help with semen quality. The fertility clinic is okay with Dan taking the fish oil, but make sure you talk about all medications and supplements you take with your own clinic.
- L-carnitine
- Acetyl l-carnitine
- CoQ10 – we have different doses
- Vitamin E
- Selenium
- Vitamin C
- Vitamin D3 – we take the same one
- Zinc
Going Forward
Since we discovered the progesterone deficit in December, we used progesterone supplements in the second half of my January cycle. Dan and I weren’t expecting me to get pregnant that cycle, but we wanted to be able to start treatment. We were also hoping to give me time to get used to it. It turns out, progesterone makes me very ill. Unfortunately, I need to continue it because it’s incredibly important for pregnancy (as I talked about in part one).

This cycle, and the next few cycles, we will do Clomid before ovulation (my protocol is ten pills taken over five days) and progesterone suppositories after ovulation. Both of the medications are no fun, but if it gets me a baby then it’s all worth it! We are also going to try IUI with at least some of the Clomid and progesterone cycles. If, after a few cycles, I’m still not pregnant, we will meet with the doctor again and figure out a new plan.
Please keep your fingers crossed and best wishes sent our way! We’re hoping that I’ll get a positive test, and that it will result in a full-term pregnancy with a living baby at the end, sooner rather than later! A year and a half of trying has been long enough for me, and I am eager to meet our someday-baby!

Good luck!!!
LikeLiked by 1 person
Thank you!
LikeLike